Cancers that metastasize, or spread from their original site to new areas of the body, are particularly challenging to treat. This is especially true in breast cancer, which can aggressively travel to other organs, worsening symptoms and complicating treatment.
Now, a new study by a multi-institutional team of scientists has revealed key differences between primary breast cancers and their metastases. The findings offer fresh insights into how metastatic breast cancer develops and progresses — and provides vital opportunities for new therapeutic approaches.

“Until now, we didn’t have a clear understanding of why breast cancers metastasize in the way they do. Our findings show that the answers lay not necessarily in genes themselves but in epigenetic changes that shape how genes are regulated,” said VAI Professor Peter W. Laird, Ph.D., one of the study’s senior authors. “This work helps us better understand the factors that drive metastasis, which is crucial for developing new ways to more effectively treat breast cancer.”
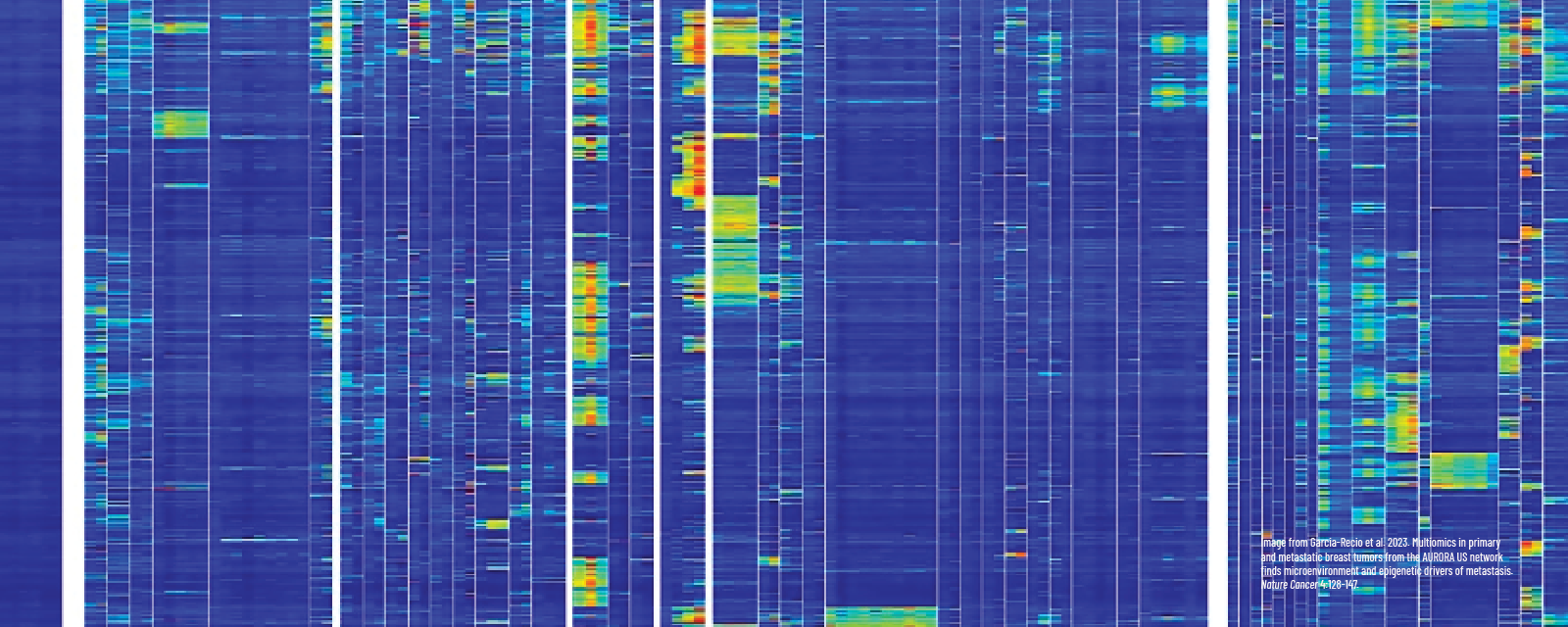
The study, published in Nature Cancer, is among the first to use an array of genetic and epigenetic tools to analyze breast cancer samples from both the cancer’s original site and paired metastases. This allowed the researchers to pinpoint the biological differences that help breast cancers spread.
One of the most prominent features is a change to the immune system that resulted in lower numbers of immune cells to attack cancer cells. This immune shift was present in 17% of metastatic breast cancer samples and arose from changes to the HLA-A gene, which plays an important part in the immune system’s ability to detect and combat abnormal cells like cancer cells.
One type of change to the HLA-A gene resulted from the addition of a chemical tag, called a methyl group, which switched the gene off. This process, called DNA methylation, is an important epigenetic process that ensures the instructions in genes are used at the right time in the right cells. When epigenetic mechanisms go awry, diseases such as cancer can result. The team also found that loss of a portion of the HLA-A gene itself had a similar effect to the epigenetic tag — a reduction in the number of immune cells available to combat cancer cells.
The study was conducted by the AURORA US Network, a collaborative team of expert scientists and clinicians who hail from institutions across the U.S. Laird led the DNA methylation analysis and is one of the study’s seven senior authors. Toshinori Hinoue, Ph.D., a bioinformatics scientist in Laird’s lab at VAI, is a co-first author of the study. VAI’s Hui Shen, Ph.D., also contributed to the findings. The project was led by Charles Perou, Ph.D., at University of North Carolina.
Research reported in this publication was supported by the Breast Cancer Research Foundation under award no. ELFF-14-002 through the Evelyn H. Lauder Founder’s Fund for Metastatic Breast Cancer Research; Vanderbilt-Ingram Cancer Center Support Grant P30CA68485 and National Cancer Institute SPORE 2P50CA098131-17 (Balko); Lineberger Comprehensive Cancer Center Grant P30-CA016086-45 and NCI Breast SPORE Program P50-CA058223 (Perou and Carey). The results published here are in whole or part based upon data from the Cancer Genome Atlas managed by the NCI and NHGRI (dbGaP accession phs000178). The RedCap instance used to capture clinical data in this project was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award no. UL1TR002489. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.