Explainer: What are mitochondria?
May 20, 2020
If you ask high school biology students about mitochondria, they’re likely to respond with the same answer: mitochondria are the powerhouses of the cell.
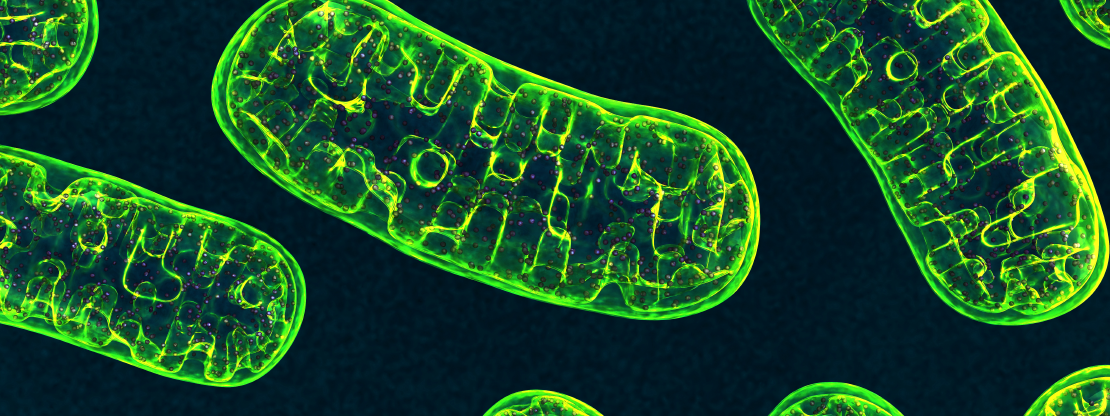
But let’s get more specific. To start, mitochondria are organelles (tiny cellular versions of organs) that generate most of the energy needed for cells to function and survive.
Mitochondria march to the beat of their own drum
Unlike other parts of a cell, replication of these power-plant organelles is not tied to cell division — mitochondria divide independently of the cell that they call home. This, among other unique features, are holdovers from ancient ancestors of mitochondria, which were likely free-living, single-celled organisms called prokaryotes.
The thinking goes that an ancient symbiosis resulted when a cell containing a nucleus (the “command centers” of certain cells) engulfed a prokaryote, which does not have its own nucleus. The host cell came to rely on the prokaryote for energy production, while the prokaryote used the host cell for protection. Over time, this relationship developed into what we see today: a cell that relies on its mitochondria for energy.
Mitochondria also have their own very small and widely varied genome — another trait carried over from their single-celled ancestors — and are generally inherited only from the mother.
How can we use our understanding of mitochondria to battle disease?
When mitochondria are not functioning properly, problems can arise that then contribute to disease — including cancers or neurodegenerative diseases like Parkinson’s.
Take cancer cells, for example, which have voracious appetites for energy. If we can find ways to turn down or stop these mitochondrial power-plants in malignant cells, we may be able to deprive the cells of the energy required to spread and, ultimately, kill them (read more about a recent study on that topic here).
Evidence also suggests that mitochondria have a role to play in the onset and progression of Parkinson’s disease, a neurodegenerative disorder for which there currently are no treatments that slow or stop progression. A wealth of recent research suggests that a breakdown in brain cells’ ability to produce energy may interfere with their “housekeeping” systems, allowing abnormal, toxic proteins to pile up, eventually killing these critical cells. The death of these cells leads to Parkinson’s hallmark symptoms, such as loss of the ability to move.
What does all of this mean for treating disease?
Many medications already exist that affect cellular energy produced by mitochondria, such as those used to treat diabetes. In fact, several medications for Type 2 diabetes are being investigated as potential therapies for cancer and Parkinson’s (read more about these efforts in cancer here and in Parkinson’s here).

