The nose knows: Understanding the link between the sense of smell and Parkinson’s
January 16, 2017

A major clue to understanding Parkinson’s and other neurodegenerative diseases may be right in front of our faces.
Or rather, on our faces.
At first blush, the nose may not be the first place many people think of when it comes to problems with the brain. However, hundreds of studies over the years have described a link between neurodegenerative diseases and a gradual loss of the ability to detect odors, to differentiate between them and even to remember them.
To tie all of these findings together, VARI’s Dr. Nolwen Rey and Dr. Patrik Brundin along with Case Western Reserve University’s Dr. Daniel W. Wesson combed through more than 500 scientific papers, developing a comprehensive look at what’s going on at a molecular level. Here are the top three takeaways from their review:
There is a solid link between sense of smell and neurodegenerative diseases.
Long before the hallmark symptoms of Parkinson’s disease set in, many people begin to lose their sense of smell. Although this effect has been documented for decades, its significance has only recently been recognized as an important early sign of the disease. And it’s not just Parkinson’s—about 90 percent of people who are eventually diagnosed with a neurodegenerative disease experience some type of problem with their sense of smell.
Exposure to environmental toxins or viruses could trigger changes in the nose.
But why are changes in the sense of smell associated with neurodegenerative diseases?
In short, proximity.
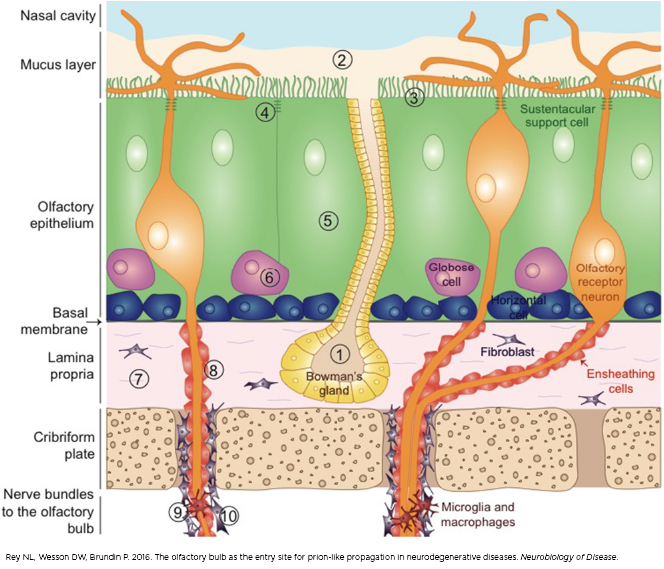
The olfactory system is far more open to the outside world, including environmental toxins and viruses, than many other systems in the body. Exposure to these factors may cause inflammation, leading to critical changes in the nose that trigger the earliest stages of neurodegeneration. In Parkinson’s, scientists think the nose is one of the sites where abnormal alpha-synuclein may first start clumping together. (There’s increasing evidence this also occurs in the gut, but that’s a story for another post).
Some neurodegenerative diseases move from the nose to the brain via clumps of proteins that jump from cell to cell.
Before clumps of abnormal proteins can impact the brain, they have to get there. Based on evidence uncovered in recent years, scientists believe the proteins move from cell to cell up the nerves that lead from the nose into the olfactory bulb and, eventually, to other areas of the brain. In Parkinson’s, it’s still unclear whether alpha-synuclein causes the cell damage and cell death that leads to symptoms or if its presence is a by-product of the disease’s spread.
Why does this matter?
As the old adage goes, know thy enemy. By better understanding how Parkinson’s and other neurodegenerative diseases get started, scientists can develop new ways to diagnose and treat these devastating disorders.
Want more information? Read the full review by Drs. Nolwen Rey, Daniel W. Wesson and Patrik Brundin here. Learn more about VARI’s Parkinson’s disease research here.
TERMS TO KNOW
Neurodegenerative disease: Any disease that involves a loss of brain function over time. These diseases include Parkinson’s, Alzheimer’s, Lewy body dementia and many others.
Alpha-synuclein: Alpha-synuclein is a protein whose role in healthy brain cells isn’t entirely clear, although it has been linked to communication between cells. Clumps of abnormal alpha-synuclein called Lewy bodies are a key feature of Parkinson’s disease.
Olfactory system: The body’s system that controls the sense of smell
Olfactory bulb: The region of the brain responsible for sense of smell
Parkinson’s disease: A progressive neurodegenerative disease that is marked by loss of voluntary movement, rigidity and stilted gait as well as a constellation of non-motor symptoms including digestive problems, cognitive decline and loss of sense of smell. An estimated seven to 10 million people worldwide have Parkinson’s.