For VAI Assistant Professor Dr. Michael Henderson, studying the brain and unraveling its mysteries is a final frontier of sorts, one that holds immense potential for treating diseases like Parkinson’s and dementia with Lewy bodies.
VAI Voice caught up with Dr. Henderson (virtually, of course) to discuss his research, what first inspired him to pursue science and the future of research and treatment for Parkinson’s and dementia with Lewy bodies.

Q: Where did you grow up?
MH: I was born in Nevada, but I have never lived in one place longer than seven years. My parents enjoyed moving around. Besides Nevada, I have lived in Tennessee, Colorado, Florida, California, Connecticut, Pennsylvania and now Michigan!
Q: When did you first become interested in science? What inspired you to study neurodegenerative diseases?
MH: I was innately curious about the world growing up, as I think most children are. The power of a good experiment to tell you something about the world without consulting a book can be exhilarating. In high school, I took an anatomy course and learned all about the organs of the body. During the lesson on the brain, it became clear how much of neuroscience was still a black box. It seemed like a final frontier to me, so I pursued neuroscience research as an undergraduate. As a graduate student, I was struck by the fact that there are no disease-modifying treatments for neurodegenerative disorders. As someone with relatives who suffer from these diseases, I felt that this was an area of research in which biomedical research could enhance millions of lives.
Q: How would you describe your research to someone without a science background?
MH: Maintaining a healthy brain is somewhat like maintaining a house. The original structure of the house is like your genes. The house may have a critical weakness (or gene mutation) that won’t matter for years. But eventually, as the house weathers storms and floods and sun and wind, the house wears down. That weakness becomes more important. The brain has a strong, redundant structure to protect it from most damage, but over time, these protections weaken and can be worsened by gene mutations. My research tries to find these weakened areas and identify a way to reinforce them so the brain can continue to function healthily into old age.
Q: Where do you think Parkinson’s research and treatment will be in 10 years? Where do you think research and treatment will be for dementia with Lewy bodies?
MH: Researchers have developed a wide variety of therapies for Parkinson’s and dementia with Lewy bodies over the past decade. It is a very exciting time for therapy because many of these treatments are entering Phase II and III clinical trials. This means that, within a few years, we will learn if these therapies can change the course of disease. We are also getting more sophisticated about how we measure disease progression. In 10 years, we will be closer than ever to disease-modifying treatments. Neurodegenerative diseases are complex and likely start decades before symptoms, so therapies may need to be started very early, or may only treat a subset of patients. That is why pursuing multiple research and treatment strategies is so critical.
Q: To date, what has been your favorite scientific accomplishment?
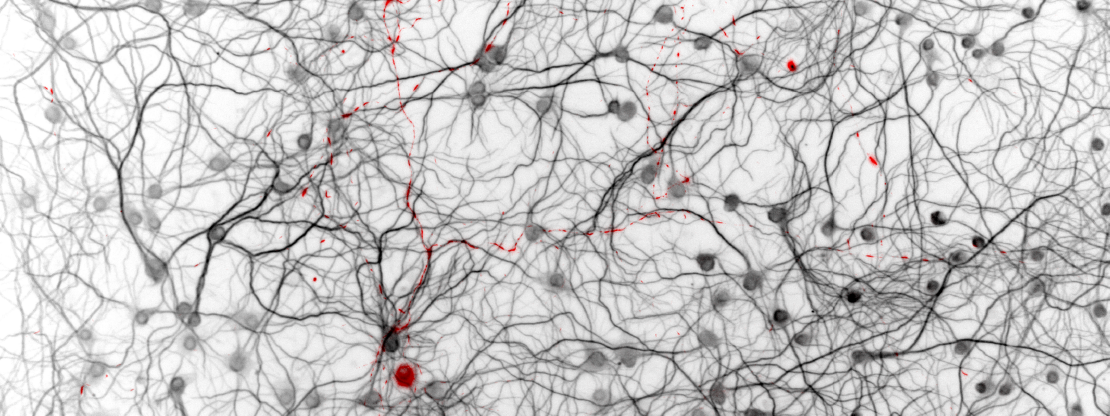
MH: Neurodegenerative diseases are progressive, meaning a patient’s symptoms generally worsen over time. We also know that misfolded proteins show up in more regions of the brain as disease progresses. There were two major hypotheses in the field about that progression. One postulated that pathology spreads through the brain from cell to cell. The other hypothesized that certain neurons were simply more vulnerable to developing pathology.
To test these hypotheses, we spent four years mapping misfolded proteins as they spread through the brain. Through computational modeling of this process, we were able to demonstrate that pathology spreads through neuron connections. But there are certain regions that are resilient to developing pathology.
We think of it like a road trip. If you were driving from Philadelphia to Grand Rapids, you would follow the roads. But if you followed a road with no gas station, you would run out of gas and travel no farther. Pathology also needs to “gas up” on its road trip, but some regions do not have “gas stations,” making those regions resilient against developing pathology. By modeling this process, we can understand how disease progresses and estimate the likely efficacy of therapies to slow that progression.
Q: What do you like to do in your free time?
MH: I have two very active children. When I have free time, I usually spend it with my wife and children hiking, riding bikes and playing games. They each have a unique perspective on the world, and it reminds me to keep an open mind in my research.
Q: What made you decide to come to VAI?
MH: Critical mass. Science is difficult, and a diversity of perspectives and technical expertise focused on similar goals is needed to move the field forward. VAI has assembled a team of world experts in neurodegenerative diseases. As an early career researcher, this critical mass of neurodegeneration researchers is especially important to help move my own research program forward.
Q: How do donors and philanthropy impact research?
MH: As researchers, it is our job to identify important research questions and design experiments to address those questions. There is sometimes a gap between the ideal theoretical experiment and what fits within the lab budget. Philanthropy can provide a valuable bridge to allow us to pursue novel and potentially fruitful research directions.
Learn more our Dr. Henderson and his research at hendersonlab.vai.org.
Want to meet other VAI scientists? Check out our series of Q&As on VAI Voice here.