Connecting the genetic dots
November 12, 2018
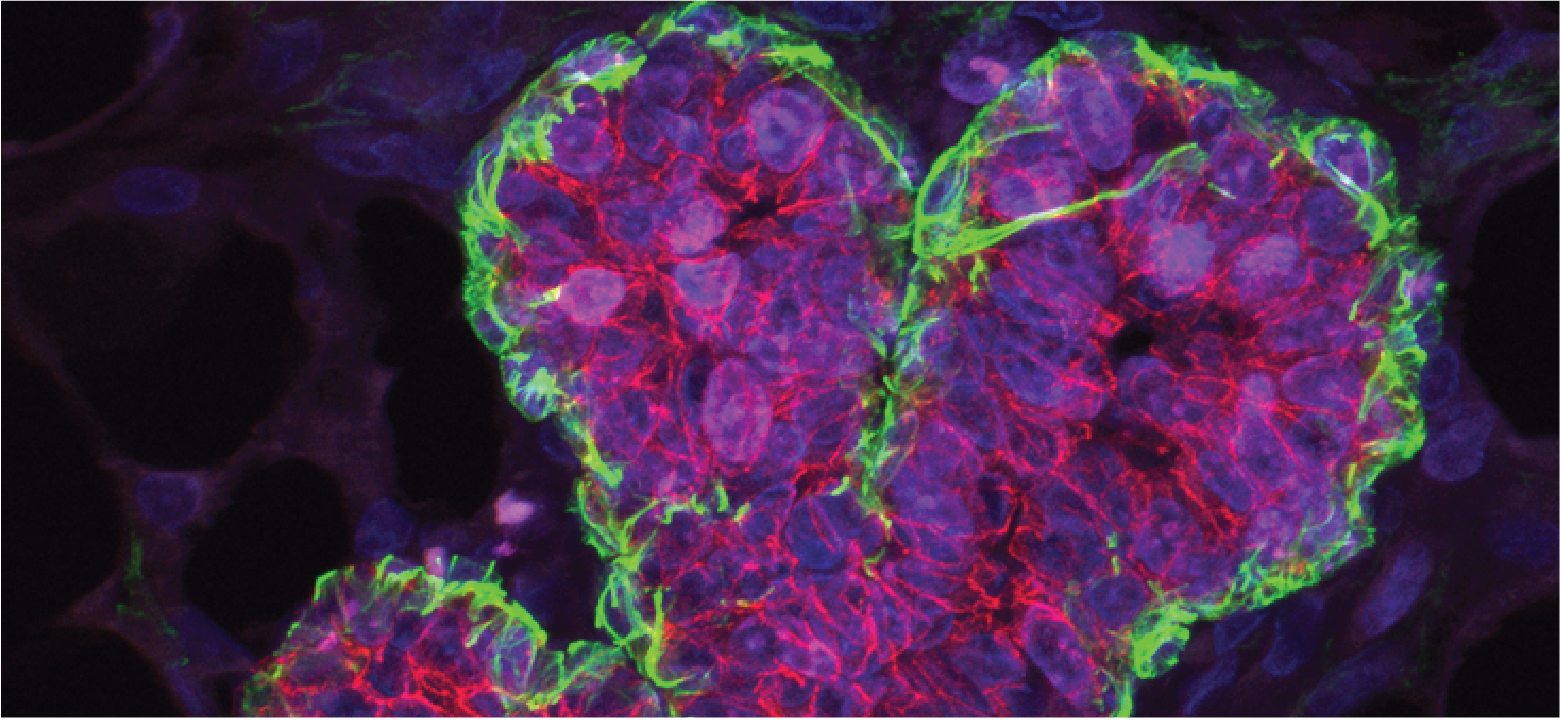
Breast cancer is the most common cancer in women. Neurofibromatosis type 1 is a rare genetic disorder. A single gene may hold answers that could lead to new treatments for both.
An aggressive breast cancer and a rare disease marked by benign tumors on the nerves and skin have a common genetic root, one that may lead to improved therapies for both conditions, according to recent findings from Van Andel Research Institute scientists.

“Rare diseases typically don’t receive as much attention because they affect a smaller number of people. Our findings are a great reminder of why it’s so important to study these disorders — the results can help people with rare diseases but also often have a much broader impact,” said Dr. Carrie Graveel, a VARI senior research scientist and breast cancer expert who led the project. “In this case, we found that NF1, the gene that causes neurofibromatosis, also greatly increases the risk of developing a particularly tough-to-treat type of breast cancer in women with and without neurofibromatosis.”
NF1 plays an important role in the body — it moderates cellular proliferation, ensuring that our tissues and organs aren’t overrun with a surplus of cells. When it malfunctions, cell reproduction spins out of control, resulting in either benign growths (such as those in neurofibromatosis) or in malignant tumors (such as cancer).
When NF1 was discovered and linked to neurofibromatosis in 1990, it was an exciting breakthrough in a disease that has largely thwarted attempts at treatment. Since then, scientists have continued combing the gene for clues in the hopes of translating their findings into new therapies that could help people around the world.
Their efforts are paying off: we now know that mutations in NF1 increase cancer risk (in fact, NF1 is one of the most commonly mutated or deleted genes in certain brain, lung and ovarian cancers).
And, even more recently, clinical evidence has suggested that NF1 elevates the risk of breast cancer, an effect that is even more pronounced in women with neurofibromatosis — below the age of 40, women with neurofibromatosis have a 10-fold increase in their risk of developing breast cancer.
Still, the fine details about the link between NF1 and breast cancer remained murky.

So Graveel and Dr. Matt Steensma, a physician-scientist at VARI and Spectrum Health and an authority on rare diseases, started digging into the data.
Together with their team, they scoured genetic information from METABRIC, a comprehensive compendium of nearly 2,000 breast cancer cases. Their findings were striking — a full quarter of cases in the database harbored a mutation in NF1, which also correlated to a marked decrease in survival.
Steensma and Graveel also found that NF1 is related to estrogen signaling in breast cancer and may play an important role in how breast cancers become estrogen-resistant. Estrogen is a critical hormone that also can fuel tumor growth.
But along with these new answers also come many new questions, Steensma said.
“Now that we’ve more firmly established the influence of NF1 on certain breast cancers, our next steps are to figure out ways to translate these findings into patient care,” he added. “There is still much more to discover that will help us on this path and, most importantly, that will help us find new, more powerful ways to help people with both of these diseases.”
This work was supported by the VARI Faculty Innovation Fund, the Breast Cancer Research Foundation and Tempting Tables.
